There are two different kinds of leg length discrepancies, congenital and acquired. Congenital indicates that you are born with it. One leg is structurally shorter compared to the other. As a result of developmental periods of aging, the brain picks up on the walking pattern and recognizes some variance. The body usually adapts by tilting one shoulder to the "short" side. A difference of under a quarter inch is not very uncommon, doesn't need Shoe Lifts to compensate and generally does not have a serious effect over a lifetime.

Leg length inequality goes typically undiscovered on a daily basis, however this condition is very easily remedied, and can eliminate a number of incidents of back problems.
Therapy for leg length inequality commonly consists of Shoe Lifts. Most are low-priced, often priced at under twenty dollars, in comparison to a custom orthotic of $200 or more. Differences over a quarter inch can take their toll on the spine and should probably be compensated for with a heel lift. In some cases, the shortage can be so extreme that it requires a full lift to both the heel and sole of the shoe.
Mid back pain is easily the most widespread ailment affecting men and women today. Over 80 million men and women experience back pain at some point in their life. It's a problem which costs businesses vast amounts of money every year on account of time lost and productivity. Fresh and superior treatment solutions are constantly sought after in the hope of decreasing the economical impact this condition causes.

Men and women from all corners of the earth experience foot ache due to leg length discrepancy. In these types of situations Shoe Lifts might be of very beneficial. The lifts are capable of alleviating any pain and discomfort in the feet. Shoe Lifts are recommended by many certified orthopaedic practitioners".
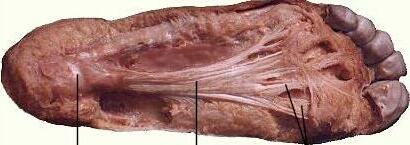
In order to support the body in a balanced manner, your feet have a critical role to play. Despite that, it can be the most overlooked zone of the body. Many people have flat-feet which means there may be unequal force placed on the feet. This causes other parts of the body like knees, ankles and backs to be impacted too. Shoe Lifts make sure that appropriate posture and balance are restored.

Leg length inequality goes typically undiscovered on a daily basis, however this condition is very easily remedied, and can eliminate a number of incidents of back problems.
Therapy for leg length inequality commonly consists of Shoe Lifts. Most are low-priced, often priced at under twenty dollars, in comparison to a custom orthotic of $200 or more. Differences over a quarter inch can take their toll on the spine and should probably be compensated for with a heel lift. In some cases, the shortage can be so extreme that it requires a full lift to both the heel and sole of the shoe.
Mid back pain is easily the most widespread ailment affecting men and women today. Over 80 million men and women experience back pain at some point in their life. It's a problem which costs businesses vast amounts of money every year on account of time lost and productivity. Fresh and superior treatment solutions are constantly sought after in the hope of decreasing the economical impact this condition causes.

Men and women from all corners of the earth experience foot ache due to leg length discrepancy. In these types of situations Shoe Lifts might be of very beneficial. The lifts are capable of alleviating any pain and discomfort in the feet. Shoe Lifts are recommended by many certified orthopaedic practitioners".
In order to support the body in a balanced manner, your feet have a critical role to play. Despite that, it can be the most overlooked zone of the body. Many people have flat-feet which means there may be unequal force placed on the feet. This causes other parts of the body like knees, ankles and backs to be impacted too. Shoe Lifts make sure that appropriate posture and balance are restored.



 Overview
Overview Symptoms
Symptoms Prevention
Prevention Overview
Overview Symptoms
Symptoms


03.jpg)
 Achilles tendinitis (or Achilles tendonitis) is a strain of the Achilles tendon, which connects the calf muscles to the heel bone. Pain can be moderate or severe, but the condition is not usually serious. Of course, if you are suffering the leg and heel pain it brings, it certainly feels serious enough.
Achilles tendinitis (or Achilles tendonitis) is a strain of the Achilles tendon, which connects the calf muscles to the heel bone. Pain can be moderate or severe, but the condition is not usually serious. Of course, if you are suffering the leg and heel pain it brings, it certainly feels serious enough.

 RSS Feed
RSS Feed